HIV cured in baby for the first time: scientists
WASHINGTON - Agence France-Presse
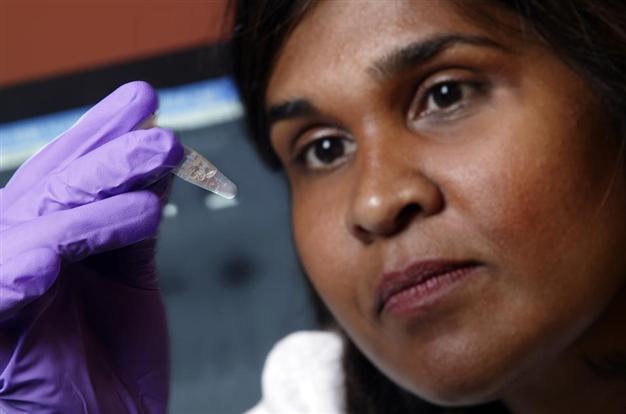
This image provided by Johns Hopkins Medicine shows Dr. Deborah Persaud of Johns Hopkins' Children's Center in Baltimore. A baby, born with the AIDS virus, appears to have been cured scientists announced Sunday, March 3, 2013, describing the case of a child from Mississippi, who's now 2½ and has been off medication for about a year with no signs of infection. If the child remains free of HIV, it would mark only the world's second known cure. Specialists say the finding offers exciting clues for
Researchers say they have, for the first time, cured a baby born with HIV -- a development that could help improve treatment of babies infected at birth.There is an important technical nuance: researchers insist on calling it a "functional cure" rather than a complete cure.
That is because the virus is not totally eradicated. Still, its presence is reduced to such a low level that a body can control it without the need for standard drug treatment.
The only fully cured AIDS patient recognized worldwide is the so-called "Berlin patient," American Timothy Brown. He is considered cured of HIV and leukemia five years after receiving bone marrow transplants from a rare donor naturally resistant to HIV. The marrow transplant was aimed at treating his leukemia.
But in this new case, the baby girl received nothing more invasive or complex than commonly available antiretroviral drugs. The difference, however, was the dosage and the timing: starting less than 30 hours after her birth.
It is that kind of aggressive treatment that likely yielded the "functional cure," researchers reported Sunday at the 20th annual Conference on Retroviruses and Opportunistic Infections (CROI) in Atlanta, Georgia.
What researchers call dormant HIV-infected cells often re-start infections in HIV-infected patients within a few weeks after antiretroviral treatment stops, forcing most people who have tested HIV-positive to stay on the drugs for life or risk the illness progressing.
"Prompt antiviral therapy in newborns that begins within days of exposure may help infants clear the virus and achieve long-term remission without lifelong treatment by preventing such viral hideouts from forming in the first place," said lead researcher Deborah Persaud, of Johns Hopkins Children's Center in Baltimore, Maryland.
It appears to be the first time this was achieved in a baby, she said.
The baby was infected by her HIV-positive mother, and her treatment with therapeutic doses of antiretroviral drugs began even before her own positive blood test came back.
The typical protocol for high-risk newborns is to give them smaller doses of the drugs until results from an HIV blood test is available at six weeks old.
Tests showed the baby's viral count steadily declined until it could not longer be detected 29 days after her birth.
The child was given follow-up treatment with antiretrovirals until 18 months, at which point doctors lost contact with her for 10 months. During that period she was not taking antiretrovirals.
Researchers then were able to do a series of blood tests -- and none gave an HIV-positive result.
Natural viral suppression without treatment is an exceedingly rare occurrence, seen in fewer than half a percent of HIV-infected adults, known as "elite controllers," whose immune systems are able to rein in viral replication and keep the virus at clinically undetectable levels.
Experts on HIV have long wanted to help all HIV patients achieve elite-controller status. Researchers say this new case offers hope as a game-changer, because it suggests prompt antiretroviral therapy in newborns indeed can do that.
Still, they said, their first priority is learning how to stop transmission of the virus from mother to newborn. ARV treatments of mothers currently stop transmission to newborns in 98 percent of cases, they say.
"Our next step is to find out if this is a highly unusual response to very early antiretroviral therapy or something we can actually replicate in other high-risk newborns," Persaud pointed out. The research was funded by the National Institutes of Health and the American Foundation for AIDS Research.
















